KETAMINE-ASSISTED THERAPY
The Science Behind Ketamine
Ketamine is a powerful medicinal tool for healing the mind.
Let’s explore the science behind its therapeutic effects.
Intro to Ketamine
Ketamine is a dissociative anesthetic initially used to sedate patients and provide pain relief and has recently gained significant attention for its remarkable potential to improve mental health conditions. Unlike traditional antidepressants, which may take weeks to show effects, ketamine can often reduce symptoms in hours or days.
-
While research is ongoing, the American Psychiatric Association and the National Institute of Mental Health have thoroughly examined the literature and confirmed that ketamine stands out as one of the most rapid-acting antidepressant medications currently available. Ketamine's unique mechanism shows that it not only provides rapid relief from conditions like depression, anxiety, and PTSD but also offers hope for individuals who have found little success with other treatments to reduce a variety of mental health symptoms that impede daily living.
How will it help me?
Past traumas or current life stressors can affect the brain’s ability to break free of unhealthy thought and behavioral patterns. Ketamine helps to re-engage the parts of the brain that are stuck in a loop of negative behaviors and restores its ability to better regulate stress and enhance mood especially when combined with psychotherapy.
How Does Ketamine Work?
Ketamine is FDA-approved as a dissociative anesthetic and was found to alleviate symptoms related to treatment resistant depression. It is also prescribed off-label to address numerous symptoms such as anxiety, PTSD, negative thought patterns, and many more. While research is ongoing, it was found to be often more effective than many anti-depressants as it targets a different neurochemical called Glutamate and works as a glutamate receptor modulator, specifically targeting the N-methyl-D-aspartate (NMDA) receptors in the brain. By blocking these receptors temporarily, ketamine enhances the production of brain-derived neurotrophic factor (BDNF) or what is commonly referred to as “brain fertilizer,” fostering neural connections and promoting neuronal growth. This process reinvigorates neuroplasticity (the brain’s ability to change) and helps repair and strengthen brain circuits associated with mood regulation and resilience.
A MEDIC AREA DESIGNED BY FOOD MACHINERY CORPORATION. JULY 28, 1969.
Credit: Cynthia Copple/Overseas Weekly Collection/Hoover Institution Library and Archives
The History of Ketamine
The origins of ketamine trace back to its formulation in the 1960s, followed by its approval by the FDA in 1970 for its potent anesthetic effects. Ketamine's exceptional safety profile, even at high doses, made it a preferred choice over other anesthetics due to its unique ability to sustain stable blood pressure and not impede respiration. Its fast-acting and dissociative properties made it valuable in emergencies and often used during the Vietnam War. Ketamine provided effective pain relief and sedation, allowing medical personnel to perform necessary procedures on wounded soldiers quickly and efficiently, even in challenging combat environments.
In 1973, the initial evidence of ketamine's antidepressant properties emerged within a university hospital's psychiatric unit. This study showcased its capacity to enhance insights into psychotherapy and alleviate mental health symptoms. Decades of research have showcased how ketamine has evolved from a conventional anesthetic to a groundbreaking mental health treatment with transformative results. Despite this, its full potential only recently came to light in the mainstream, as increasing studies confirm its effectiveness in various mental health applications.
The Neurobiology of Ketamine
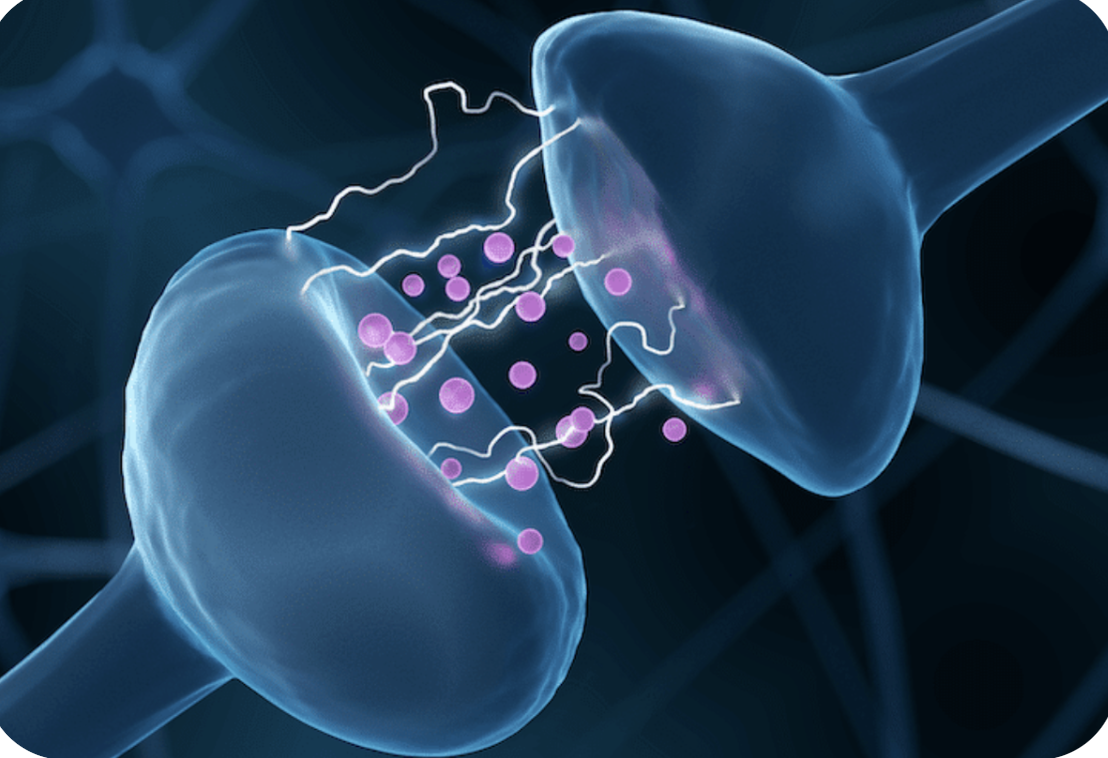
When we feel anxious or depressed, this mental stress weakens the links between our brain cells, impacting learning, memory, and mood regulation, which makes it hard to cope with life’s challenges. Ketamine helps restore the ability for new neural connections to occur to regain the ability to create healthier thought patterns, increase the ability for better mood regulation and most often have instant antidepressant effects.
-
The efficacy of ketamine in producing powerful antidepressant effects, especially in cases where traditional antidepressants have failed, stems from its unique mechanism of action. Unlike conventional antidepressants that primarily target the serotonin, dopamine, and norepinephrine systems, ketamine operates by blocking the NMDA receptor and triggers the release of glutamate, a neurotransmitter. This release activates pathways that promote the release of growth factors, such as BDNF, which facilitate the growth of new synapses and establish healthier and stronger connections between neurons, resulting in neuroplasticity, or the brain's ability to adapt and learn in response to new stimuli and circumstances.
Ketamine can also help stop negative thought patterns. Neuroimaging has shown that the brain's Default Mode Network (DMN) gets suppressed by ketamine, which allows a break from the constant rumination of worry and doubt. This pause enables new insights to emerge, leading to personal growth.
By priming the brain for new learning and interrupting negative thought patterns, ketamine helps reset neural networks, facilitating the acquisition of further information, behavioral patterns, and insights at a neurobiological level. This impact could explain why ketamine accelerates the process of psychotherapy and fosters lasting and meaningful changes during ketamine-enhanced sessions.
One study involving mice, funded by the National Institute of Mental Health, showed that when exposed to a stressor, the connections between brain cells were reduced, which contributed to depression-related behaviors. (As seen in the image below.) However, the study showed that even one dose of ketamine can restore connections between brain cells in the prefrontal cortex, a region associated with depression. The study also revealed that newly formed brain connections, called dendritic spines, play a crucial role in sustaining the antidepressant effects of ketamine. Deleting these spines led to the return of depression-related behaviors. These findings have paved the way for interventions promoting lasting depression remission in humans, offering hope for better management of mood disorders.
Photo Credit: Science
In mouse nerve cells, dendritic spines (shown by red arrows in the top panel) vanished after a stressor of corticosterone treatment (middle panel). However, after the mice received a ketamine shot, some of these spines regrew (indicated by blue arrows in the bottom panel). Science 2019, DOI: